Key Takeaways
- Accurate data migration prevents denied claims and payment delays.
- Clearinghouse transitions can cause cash flow disruptions if mishandled.
- Proper staff training reduces speech therapy billing errors and ensures revenue continuity.
- Explore billing services specifically designed for speech-language pathologists.
Have you ever upgraded your computer expecting a better experience—only to discover missing programs, broken apps, and inconvenient glitches? Now imagine that same disruption—but in your speech therapy billing department.
Adopting a new EHR system is an exciting step, and should be one your SLP practice is looking forward to. The right platform can streamline charting, improve clinical documentation, and boost clinical compliance. But without strategic planning, transitions can introduce errors, claim denials, and serious revenue leakage—particularly when speech therapy billing codes, like CPT code 97129, are involved.
Whether you’re transitioning from paper charts to digital records or switching between EHR systems, speech therapy billing codes and reimbursement rates demand special attention—especially if you want to avoid these five common billing pitfalls during the process.
Table of Contents
1. Overlooking Data Migration and Billing Validation
The transition to a new EHR introduces major risks if billing data isn’t migrated and validated properly. In speech therapy, missing or corrupted records can derail CPT coding and lead to cascading issues—like delayed reimbursements, denied claims, and inaccurate patient balances. This can disrupt your revenue cycle and negatively impact your bottom line in both the short and long term.
Many SLPs underestimate the complexity of migrating key billing data—such as historical CPT code entries (e.g., 92521, 97129), insurance authorizations, payer contracts, aging reports, and ICD-10 mappings. In reality, over one third of transitions get held up. A 2022 JAMIA study found that nearly 38% of EHR data migration projects experience delays or go over budget due to incomplete planning.
How to Avoid It
Work with an EHR platform designed for speech-language pathology, like SpeechTherapy-Cloud, to build a comprehensive migration strategy that includes billing-specific elements such as CPT codes, payer fee schedules, aging reports, and prior authorization records.
Before fully launching the new system, perform controlled testing by submitting sample claims—including high-volume SLP codes like 97129 or 92523—to confirm data accuracy. Conduct internal audits that compare balances and transactions between systems, and initiate your go-live in phases to reduce risk, starting with a limited number of live claims before scaling up.
2. Missing Key Steps in Your Clearinghouse Transition
An often-overlooked aspect of an EHR switch is the clearinghouse setup. Many speech therapy practices rely on integrated clearinghouses for submitting claims, receiving electronic remittance advice (ERA), and managing payment posting. Disruptions during clearinghouse reconfiguration can delay revenue and create backlogs.
According to the American Medical Association, breakdowns in health information exchange during EHR transitions can significantly impact communication, especially across third-party systems.
If your clearinghouse enrollment or payer linkages aren’t properly updated, your new EHR might start producing rejected claims—even for routine services like CPT 92507 (speech therapy, individual) or 92607 (AAC evaluation).
How to Avoid It
Notify every payer about your EHR transition at least 30 days prior to going live, and confirm that your new clearinghouse setup can support all existing payer connections. Review all enrollment documents and ensure that your ERA pathways, claim submission formats, and NPI associations are correctly mapped in the new system.
Your EHR vendor and clearinghouse should run connectivity tests before launch to prevent breakdowns. During the initial weeks post-launch, closely monitor submission status and reimbursements to detect any transmission failures or coding mismatches that could delay cash flow.
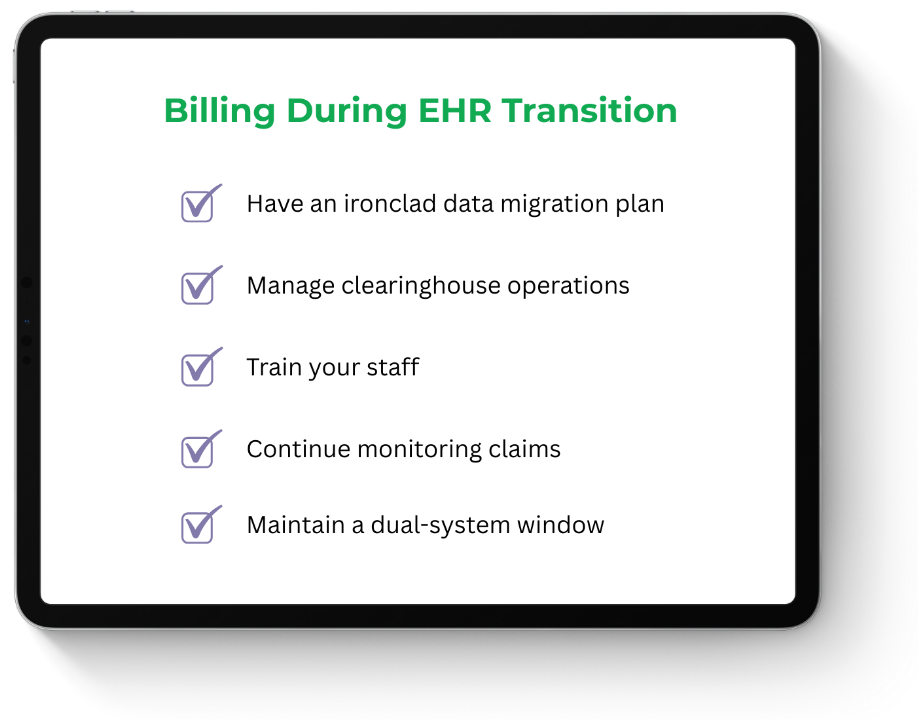
3. Undertraining Staff on Speech Therapy Billing Workflows
Even the best speech therapy EHR system can fall short if your staff isn’t equipped to use it correctly. Common training gaps—like incorrect use of CPT code 97129 (cognitive function interventions), failure to apply modifiers, or confusion around documentation prompts—can lead to underbilling, denied claims, and compliance violations.
If you’re an outpatient speech therapy, precise code usage is especially important due to frequent policy updates and payer-specific requirements (e.g., session time minimums for time-based codes like 97129/97130).
Remember, undertrained staff can derail your billing process. Your billing team, whether in-house or an SLP billing partner, must understand how to properly apply CPT code speech therapy entries to ensure accurate reimbursement and avoid claim denials during an EHR transition.
How to Avoid It
Invest in a tailored training program for each role—front desk, clinicians, and billers—with special emphasis on time-based codes, modifiers, and documentation required for reimbursement.
Partner with your EHR vendor to deliver hands-on workshops and scenario-based training that reflect the nuances of speech therapy billing, including services like swallowing therapy or speech-generating device programming. An intentional plan can help you establish a team of internal super-users to support others and build consistency.
As with any successful learning management strategy, consider implementing periodic knowledge checks to keep your team updated on compliance and insurer rules.
4. Letting Active Claims Slip Through the Cracks
In the chaos of switching systems, it’s easy to overlook claims that were already in flight. However, failing to track and manage these can result in missed follow-ups, expired timely filing windows, or unrecovered revenue.
Even small mismatches in new claim templates, diagnosis-to-CPT code logic, or billing rules can result in silent denials. For example, if a system defaults to CPT 92507 but doesn’t support the linked ICD-10 code for a specific patient condition, the claim could be rejected. This means lost revenue for your practice.
How to Avoid It
Assign designated billing personnel to monitor claims in both the legacy and new EHR systems during the transition. They should compare claims data, reimbursement rates, and denial reasons across both platforms.
Your billing team can use analytics tools to identify variances in rejection rates or reimbursement levels to further track claims. Establish a formal denial management workflow to quickly address anomalies and resolve rejections, and make sure issues are escalated promptly, especially if recurring problems surface in the new system.
5. Foregoing a Dual-System Window
A smart transition to a new speech therapy EHR isn’t a blind leap of faith. It involves a carefully plotted timeline that includes keeping your legacy system until the new one is up and running. Turning off your old EHR too soon can result in a loss of access to vital patient and claim data—especially for post-payment audits, legacy denials, or secondary insurance follow-ups.
Some practices assume the new system is ready and decommission the old one immediately, only to find themselves scrambling to retrieve critical details on prior authorizations, claim resubmissions, or historical documentation for services.
How to Avoid It
Maintain both your old and new EHR systems concurrently for at least 60 to 90 days after launch. This overlap provides a safety net for verifying historical claim data, responding to audit requests, or correcting older denials that may still be pending.
Communicate with your team, sharing clear policies for accessing legacy data, and consider keeping read-only access to the old platform for an extended period—even beyond the initial transition—especially if payer audits or state Medicaid documentation requirements are common in your practice.
Create a Plan for a Smooth Transition
Switching EHRs doesn’t have to disrupt speech therapy billing codes and reimbursement rates. With the right planning, your practice can make a seamless move—without losing revenue or productivity.
By avoiding these five costly billing mistakes and partnering with a specialty EHR like SpeechTherapy-Cloud, you can protect your revenue during the transition and ensure compliance with speech therapy-specific coding rules.